In the current study, the team explored the effectiveness of an atypical antipsychotic medication called lurasidone in 485 patients with bipolar disorder struggling with an episode of major depression (also known as bipolar depression). People living with bipolar disorder experience extreme mood swings with periods of mania alternating with depression.
Participants in the six-week study were randomly assigned to take lurasidone (some taking 20-60 milligrams per day and others 80-120 milligrams) or a placebo pill. At the time of the study, neither participants nor the scientists leading the research knew who was receiving the active drug versus the placebo.
As a group, participants who received lurasidone during the six week study period showed reduced depression compared to participants who received placebo. However, when researchers took pre-treatment CRP levels into account, a striking pattern emerged. In participants with higher levels of pretreatment CRP, lurasidone produced a large antidepressant benefit when compared to a placebo, whereas in participants with low levels of CRP, lurasidone showed no advantage over the placebo. If confirmed in future studies, these findings suggest that clinicians may be able to use a simple, inexpensive and widely available CRP blood test to determine which patients with bipolar depression could potentially benefit from the drug.
The fact that a person’s immune system may shape mental health reflects a more systemic understanding of the body compared to typical approaches in mental health practice and research.
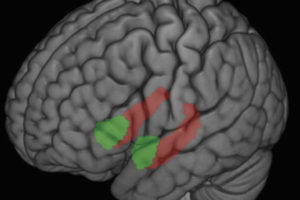
“This is part of a larger scientific story that’s emerging,” Raison says. “Inflammation affects brain functioning in ways that make us less available for social connection, which makes sense because we all tend to retreat when we feel sick. So when the body’s alarm system is telling us we’re sick, we tend to withdraw even if the threat is psychological instead of physical.”
One limitation of the study, Raison says, is that it was not designed to see if CRP would predict people’s responses; rather the larger goal was to understand if the drug in question helped treat bipolar depression. However, there were several strengths to the design, including a focus on a large patient sample and adherence to the rigorous standards required for studies designed to obtain Food and Drug Administration approval for medication use.
In the future, Raison and colleagues hope to design studies that can more specifically predict the effectiveness of interventions based on CRP levels. Raison and others hope to lead research to better understand this connection and whether CRP or other biomarkers may be predictive of how people respond not just to medications, but to other interventions as well, including mind-body approaches such as mindfulness meditation.
This research was conducted in collaboration with Sunovion Pharmaceuticals, Inc., which manufactures lurasidone. Raison reports that in the prior 12 months he has served as a consultant for Novartis, Alkermes, Shire, Usona Institute, Emory Healthcare and North American Center for Continuing Medical Education.
-Marianne Spoon