Meditation can change the way a person experiences pain, according to a new study by Center for Healthy Minds neuroscientists.
The researchers found during a pain experiment, expert meditators felt the discomfort as intensely as novice meditators, but the experience wasn’t as unpleasant for them.
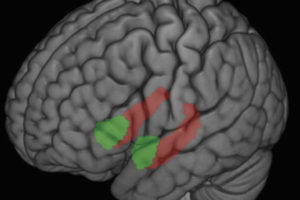
Images of brain regions linked to pain and anxiety may explain why. Compared to novice meditators, experts had less activity in the anxiety regions.
Not only did the experts feel less anxiety immediately before pain stimulation, they also became accustomed to the pain more quickly after being exposed repeatedly to it.
The scientists, based at the Center and Waisman Laboratory for Brain Imaging and Behavior, run a robust program analyzing the effects of meditation. The new study adds to a growing body of knowledge in the young field.
The study involved an advanced form of mindfulness mediation called "open presence," but other kinds of meditation also may provide benefits, says Antoine Lutz, first author on the paper appearing recently in NeuroImage.
“We predict that mindfulness-based stress reduction and related programs should also lead to a decrease in some of the elaborate brain processes that account for distress as people deal with pain,” he says.
People use many different strategies to handle pain, including trying to avoid it (blocking it out with music, for example), redefining it (“It’s not so bad today”) and changing the context of the experience (with hypnosis or a placebo pill).
Mindfulness meditation, which stresses attention to the present moment, has proven to be useful for chronic pain, but the UW researchers were interested in understanding the brain mechanisms underlying it.
They collected a group of 14 expert meditators who had meditated at least 10,000 hours and practiced open presence, which aims to cultivate an effortless, open and accepting awareness of whatever is occurring at the moment. Members of the control group had no previous experience with any type of meditation, but were given instructions on how to meditate and told to practice seven days before the test.
The test involved the application of heat to inside the forearm below the wrist. Participants were instructed to indicate when the level reached 8 on a scale of 1-10, then the heat was lowered. In each trial, subjects were given 45 seconds to settle into a meditation state, then were presented with warm heat, a cue that the real heat was coming. Immediately afterwards, participants’ brains were scanned with a functional MRI.
The scans showed during the pain application, experts had stronger activity than novices in the dorsal anterior insula and the anterior mid-cingulate, parts of a brain network sensitive to “saliency.”
“Saliency refers here to the internal or external information that is the most important at any given moment for the organism or person,” Lutz says. “Increased activation of the saliency network made the pain seem more vivid for experts than novices.”
Immediately before the delivery of pain, the experts had less activity in the saliency network and in the amygdala, an anxiety-related area, compared to novices.
“The pain didn’t bother the experts as much as it bothered the novices, in whom the anxiety of anticipation was stronger,” Lutz says.
"We predict that mindfulness-based stress reduction and related programs should also lead to a decrease in some of the elaborate brain processes that account for distress as people deal with pain."
Finally, experts had faster “neural habituation” to pain and its anticipation than novices. Habituation is a form of learning in which repeated exposure to a stimulus results in a decreased response.
Pain had a lower overall impact on the experts because they had less anxiety related to anticipation and they habituated to the pain more quickly, Lutz says.
The findings help explain how opening to pain, rather than avoiding it, can reduce the anxiety that can worsen the experience of pain.
“The goal would be to change your relationship to the pain, rather than changing the experience itself,” Lutz says.
Co-authors on the study were Daniel F. McFarlin, David M. Perlman, Tim V. Salomons and Richard J. Davidson.
This work was supported by grants from the National Center for Complementary and Alternative Medicine (U01-AT002114 to A.L. and P01-AT004952 to A.L. and R.J.D.), the National Institutes of Mental Health (P50-MH069315 to R.J.D.), and a core grant to the Waisman Center from the National Institute of Child Health and Human Development (P30-HD03352, to M. Seltzer), and gifts from Bryant Wangard and Ralph Robinson, Keith and Arlene Bronstein, the Mental Insight Foundation, and the JohnW. Kluge Foundation (to R.J.D.). David Perlman was supported by NIH training Grant T32-MH018931, R.J.D. director. Tim Salomons was supported by a Clinician-Scientist award from the University of Toronto Centre for the Study of Pain.