MADISON – In the mid-20th Century, new evidence showed that the brain could be “plastic,”and that experience could create changes in the brain. Plasticity has been linked to learning new skills, including spatial navigation, aerobic exercise and balance training.
Yet it’s remained an open question if mindfulness interventions, like meditation, can alter the brain’s structure. Some research using the well-known eight-week Mindfulness-Based Stress Reduction (MBSR) course indeed suggested so. However, this study was limited in scope and technology and perhaps skewed by elective participant pools.
In new research, a team from the Center for Healthy Minds at the University of Wisconsin–Madison, led by Richard J. Davidson, found no evidence of structural brain changes with short-term mindfulness training.
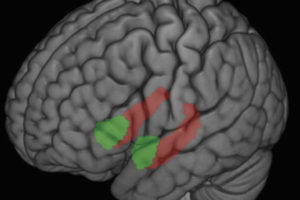
Published May 20 in Science Advances, the team’s study is the largest and most rigorously controlled to date. In two novel trials, over 200 healthy participants with no meditation experience or mental health concerns were given MRI exams to measure their brains prior to being randomly assigned to one of three study groups: the eight-week MBSR course, a non-mindfulness-based well-being intervention called the Health Enhancement Program (HEP), or a control group that didn’t receive any type of training.
The MBSR course was taught by certified instructors and included mindfulness practices such as yoga, meditation and body awareness. The HEP course was developed as an activity that is similar to MBSR but without mindfulness training. Instead, HEP engaged participants in exercise, music therapy and nutrition practices. Both groups spent additional time in practice at home.
Following each eight-week trial, all participants were given a final MRI exam to measure changes in brain structure. Data from the two trials were pooled to create a large sample size. No significant differences in structural brain changes were detected between MBSR and either control group.
“it may be that only with much longer duration of training, or training explicitly focused on a single form of practice, that structural alterations will be identified.”
Participants were also asked to self-report on mindfulness following the study. Both those in the MBSR and HEP groups reported increased mindfulness compared with the control group, providing evidence that improvements in self-reported mindfulness may be related to benefits of any type of wellness intervention more broadly, rather than being specific to mindfulness meditation practice.
So what about the prior study that found evidence of structural changes? Since participants in that study had sought out a course for stress reduction, they may have had more room for improvement than the healthy population studied here. In other words, according to the lead author of the new study, Behavioral Scientist Tammi Kral, “the simple act of choosing to enroll in MBSR may be associated with increased benefit.” The current study also had a much larger sample size, increasing confidence in the findings.
However, as the team writes in the new paper, “it may be that only with much longer duration of training, or training explicitly focused on a single form of practice, that structural alterations will be identified.” Whereas structural brain changes are found with physical and spatial training, mindfulness training spans a variety of psychological areas like attention, compassion and emotion. This training engages a complex network of brain regions, each of which may be changing to different degrees in different people, making overall changes at the group level difficult to observe.
These surprising
results ultimately underscore the importance of scrutiny for positive
findings and the need for verification through replication. In addition,
studies of longer-term interventions as well as ones singularly focused
on meditation practices may lead to different results. “We are still in
the early stages of research on the effects of meditation training on
the brain and there is much to be discovered,” says Davidson.
This work was supported in part by National Institutes of Health grants P01AT004952, P50-MH084051, R01-MH43454 and U24-AT011289 (RJD), T32MH018931 (RJD, TK), P30 HD003352-449015 and U54HD090256, grants from Fetzer Institute (RJD), John Templeton Foundation (RJD) and a National Academy of Education/ Spencer Foundation postdoctoral fellowship (MJH).
- Heather Harris