Raising the body temperature of depressed volunteers to the equivalent of a mild fever improved their symptoms of major depression for as long as six weeks after a single treatment, results from a new study show.
Researchers led by Center for Healthy Minds Professor Charles Raison conducted a small, double-blind trial to test whole-body hyperthermia as a novel treatment for major depression.
They evaluated the depressed volunteers on the Hamilton Depression Rating Scale (HDRS) and found that 60 percent of them had a response and 40 percent met the criteria for remission of depression during at least one assessment after having received the treatment.
“Our hope is to find better and faster-acting treatments for depression than the antidepressants currently in use,’’ says Raison. “We think that using heat to stimulate the skin activates serotonin-producing cells in the mid-brain, which then produce a change in how the brain functions. In a way, one might think of this pathway from the skin to the brain as a deep-brain stimulator crafted by evolution. We tap into this pathway because heat makes the brain feel happy.”
Raison announced the results today at the 2016 Meeting of the Society of Biological Psychiatry in Atlanta. The results were published online today in JAMA Psychiatry.
The researchers used a whole-body hyperthermia device to raise the body temperatures of 16 volunteers to 38.5 Celsius, the equivalent of about 101.3 degrees Fahrenheit. Another 14 were randomized to a “sham” procedure that had them lie inside the hyperthermia device with fans and lights, but only a small amount of heat, not the intense infrared heat that produced the full treatment.
“Our sham intervention was so realistic that most of the participants (10 of 14) thought they were receiving the real treatment,’’ says Raison. That is important, because it suggests the antidepressant response was not due primarily to placebo factors associated with the treatment.
The real hyperthermic treatment improved depression scores by a mean of 5.67 points more than the sham at week one and a mean difference of 4.83 points at six weeks after the treatment. The HDRS rates scores of 0 to 7 to be normal, 8 to 13 to indicate mild depression, 14 to 18 to indicate moderate depression and 19 and above to indicate severe and very severe depression.
Researchers screened 338 volunteers and wound up with 34 patients with HDRS scores of 16 and above. The two arms began with 17 volunteers each, but with dropouts, 15 wound up completing the whole-body hyperthermia and 14 the sham treatment.
Those receiving the active treatment were in a type of tent, and were heated on their chest by infrared lights and on their legs with infrared heating coils. After their body core temperature reached 38.5 degrees Celsius (usually after about an hour and half) the heat was turned off and they were allowed to cool for an hour.
"We tap into this pathway because heat makes the brain feel happy."
A week after treatment, researchers who were blinded to whether the volunteers had the real treatment or not assessed their depression levels using HDRS. Further assessments were made at two, four and six weeks. Self-reports also showed lessening of symptoms, although not as dramatic. Both groups reported only mild adverse effects.
“We were surprised to see that the effect (of reduced depression symptoms) was still present six weeks after the initial treatment,’’ Raison says.
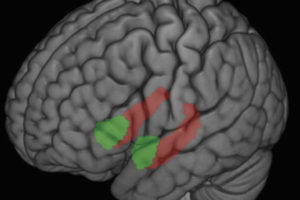
Co-author Christopher Lowry, associate professor of integrative physiology at the University of Colorado-Boulder, showed in an earlier study that whole-body heating activates neurons in the brain that synthesize the neurochemical serotonin, an effect that is shared by antidepressant drugs. In addition, Lowry said, “We know that warming the skin activates areas of the brain where activity is low in depressed patients.”
One brain area activated by heating the skin, the medial orbitofrontal cortex, is involved in the regulation of mood. This area of the brain responds to pleasant sounds, smells, images, tastes and other stimuli. A premise of the research is that certain sensory pathways evolved to mediate antidepressant-like responses. Lowry says depression is associated with over-activity of the brain’s default-mode network, which is engaged when a person is ruminating.
But throughout evolution, certain conditions made such a state of mind “extremely maladaptive,” Lowry observes. Extreme heat would demand that people shift their attention from internal thoughts to the external world.
Raison says that the current study extends results from an earlier open-treatment study his group did in Switzerland in inpatient volunteers with major depression. Hyperthermia has been used for many years, primarily in Europe, as part of a cancer-fighting regimen, although whole-body hyperthermia to treat cancer typically raises the body temperature to temperatures much higher than used in the depression studies.
According to Raison, the results of the small study are encouraging, but he cautions that because the sample size was small, more research is needed to determine how hyperthermia should be optimally delivered in terms of the temperature used and the amount of time patients are exposed to the heat. Additionally, the results may have been confounded by volunteers’ expectations that the treatment would work.
The study was conducted at the University of Arizona and funded by the Brain & Behavior Research Foundation, the Depressive and Bipolar Disorder Alternative Treatment Foundation, the Institute for Mental Health Research, the Braun Foundation and Barry and Janet Lang and Arch and Laura Brown.
–From UW-Madison School of Medicine and Public Health; Clint Talbott, communications director at CU-Boulder’s College of Arts and Sciences, contributed to this report.