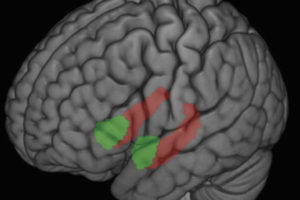
It has long been known that the part of the brain called the amygdala is responsible for recognition of a threat and knowing whether to fight or flee from the danger.
Now, using functional magnetic resonance imaging, or fMRI, scientists at the Center for Healthy Minds at the University of Wisconsin–Madison Waisman Center are watching the duration of the amygdala response in the brains of healthy people when exposed to negative images. How long the recovery takes may be an indicator of personality traits like neuroticism.
Recently published in the journal Social Cognitive and Affective Neuroscience, the study specifically examines how the amygdala responds and recovers from negative stimuli. One of the more primitive parts of the mammalian brain, the amygdala is central to processing emotion, including activating changes in the body that often accompany emotion. In terms of its evolutionary function, this region of the brain is part of a circuit that is key to our sense of fear recognition and alertness to danger.
While the role of the amygdala has been understood and well documented, the time course for the response-recovery process has never been investigated, nor observed, until the recent advance of fMRI analysis methods.
“Past studies looking at the temporal unfolding of emotional responses have focused on reports of emotional experience obtained from interviews and questionnaires,” says Tammi Kral, research specialist at the Center and an author of the paper. “This study is different because it looks at the temporal activity in the brain via fMRI.”
Through the lens of fMRI, scientists can measure the activation in the amygdala as it reacts to negative stimuli, and the subsequent recovery after the stimulus ends. This study shows that while the initial reactivity of the amygdala does not predict personality traits, a sluggish response-recovery time may be a predictor of neuroticism.
“People’s responses to negative emotional stimuli, and their ability to regulate those responses, can be a major factor in depression, anxiety and other psychological disorders,” says Kral. “In the case of depression, the person is often ruminating, perseverating – they’re unable to let go of the negative experience.”
The study could have clinical applications because it implies that changing the way people recover from negative occurrences may be a good way to improve their emotional well-being. Research from other groups also supports the idea that individual differences in emotional recovery affect overall well-being.
"People’s responses to negative emotional stimuli, and their ability to regulate those responses, can be a major factor in depression, anxiety and other psychological disorders."
A separate study has shown that subjects who use a process called reappraisal show less activity in the amygdala, for example. These people are taught to recast a negative image in a more positive way, making it less emotionally charged. Meditation may be another way to affect the activity of the amygdala.
“Our study is part of a larger effort comparing the response-recovery in the amygdalae of experienced meditators versus those in people who do not practice meditation,” she says.
Meditation practices such as mindfulness train the meditator to be open and accepting of thoughts as they arise, and then let them go without continuing to focus on them. The study suggests that the ability to recover more quickly from emotion may have a large impact on mental health. Thus, the practice of “letting go” of negative emotion can play a major role.
“I think this is important because we’re getting biological evidence of emotional recovery to complement more subjective evidence from questionnaires, and it’s giving us more information about the fundamental nature of human emotion,” Kral says.
Scientists at the Center conduct rigorous scientific research on healthy qualities of mind such as kindness, compassion, forgiveness and mindfulness. The first author on the paper was Brianna Schuyler; others were Jolene Jacquart, Cory A. Burghy, Helen C. Weng, David M. Perlman, David R.W. Bachhuber, Melissa A. Rosenkranz, Donal G. MacCoon, Carien M. van Reekum, Antoine Lutz and Richard J. Davidson.
The work was funded by the National Center for Complementary and Alternative Medicine (NCCAM) P01AT004952 to Richard Davidson, grants from the National Institute of Mental Health (NIMH) R01-MH43454, P50-MH084051 to Richard Davidson, grants from the Fetzer Institute and the John Templeton Foundation to RJD, and a core grant to the Waisman Center from the National Institute of Child Health and Human Development [P30 HD003352-449015]. BSS was supported by a Neuroscience Training Program training grant [T32GM007507; Tom Yin PI] from the National Institute of General Medical Sciences.
– Jill Ladwig